Inflammation
Many years ago, a Time magazine cover exposed the dangers of inflammation to the world, pointing out that it could lead to everything from heart attacks and strokes to Alzheimer’s disease and cancer. Since 2004 the body’s potentially treacherous self-defense mechanism has been linked to even more diseases, prompting many to suggest that inflammation may be the root cause of most human illnesses. But much of the evidence has been circumstantial, particularly around the claims that inflammation causes cancer. Scientists knew from various crime scenes left by human disease that inflammation was often present, so it must be a villain in some way, but they couldn’t find the forensic evidence to firmly pin the blame on it.
We now have that evidence. And inflammation may be even more deadly than we thought. Just in the last few months science has discovered:
- The precise mechanism by which inflammation may cause cancer.
- Proved that inflammation resulting from a skin wound may increase your risk of melanoma.
- Inflammation may be the reason diabetes and heart disease are linked, because of the inflammatory damage to blood vessels caused by high blood sugar.
- Chronic inflammation may be one of the main reasons — if not themain reason — we age.
How is it that something that’s designed to protect us can also turn against us?
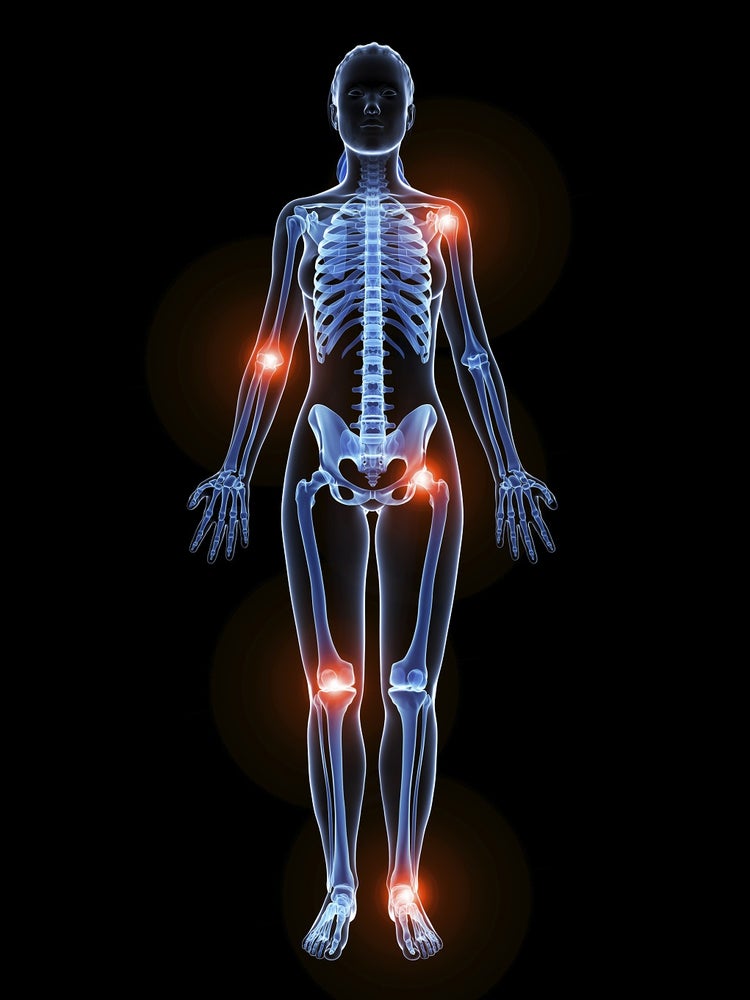
THE BODY’S CHEMICAL WARFARE
First, a quick explanation of what inflammation is: a response by our immune system to what it thinks is any attack by bacteria, viruses, toxins and other irritants. When a part of you is sore, red and swollen, that’s the immune system blasting the infected area with a range of proteins and chemicals that are designed to destroy the invaders and any damaged cells and then clean up the mess. It’s basically chemical warfare, and our immune system is really, really good at it.
In a world in which we’re constantly under attack from viruses, pathogens, toxins and other irritants and stresses, the human immune system has evolved to achieve victory without compensation for the collateral damage to healthy cells nearby. That damage can have catastrophic results for us. It also appears the immune system is extremely trigger-happy, and it will keep on waging low-level chemical warfare as long as it detects any kind of threat to our well-being regardless of whether we are aware of it or not.
Chronic or systemic inflammation is increasingly regarded as one of the biggest threats we face, and it’s particularly alarming because in many cases it’s the immune system responding to irritants from our Western lifestyle rather than invading pathogens. We may be fine with eating lots of refined foods or sugar, but our immune system isn’t. We may be cool with surviving on little sleep but our immune system isn’t. Many of us may be okay with being sedentary, but our immune system doesn’t like it. Many researchers claim it’s the massive disconnect between our Western lifestyle and our immune systems that may be responsible for much of modern disease.
THE LINK TO CANCER
Until this year we suspected that inflammation probably led to some cancers, but the precise mechanism underpinning this wasn’t clear. This mechanism was recently discovered by researchers at the Massachusetts Institute of Technology.
In a paper published in Proceedings of the National Academy of Sciences, the researchers revealed how the response by the immune system to fight off infection can create DNA mutations that lead to cancer. According to the MIT researchers, the immune system attacks invaders with a number of reactive molecules designed to neutralize it, including hydrogen peroxide, nitric oxide and hypochlorous acid. However, these molecules can also cause collateral damage to healthy tissue around the infection site.
“The presence of a foreign pathogen activates the immune response, which tries to fight it off, but in this process it also damages some of the normal cells,” points out Bogdan Fedeles, a research associate in the Department of Biological Engineering at MIT, and the paper’s lead author.
MIT research has found that some molecules generated by the inflammatory response to attack invaders, also led to “lesions” or damage in the structure of DNA in normal surrounding cells.
The specific lesion, 5-chlorocytosine (5ClC) was a damaged form of the normal DNA base cytosine. “In all cases we found that 5ClC is mutagenic, and causes the same kind of mutations seen within cells,” Fedeles says.
“That gave us confidence that this phenomenon would in fact happen in human cells containing high levels of 5ClC.”
Studies of tissue samples of patients suffering from inflammatory bowel disease have also found significant levels of 5ClC, Fedeles adds, further establishing the link between inflammation and cancer.
INFLAMMATION IN SKIN WOUNDS AND CANCER
Incredibly even the inflammatory response to a skin wound has been shown to promote cancer if there happened to be pre-cancerous cells nearby. Researchers in the United Kingdom and Denmark have shown that neutrophils — protective inflammatory
cells that are part of the body’s immune system — can divert from an induced wound to any nearby precancerous skin cells. The newly arrived neutrophils cause rapid division of these skin cells, which may cause them to progress to melanoma.
In the study published in The EMBO Journal, EMBO (European Molecular Biology Organisation) member Paul Martin, professor at Bristol University and the University of Cardiff, says, “our results provide direct visual evidence of a physical link between wound-associated inflammation and the development of skin cancer.”
The researchers were also able to show that a specific type of signaling molecule released by neutrophils, prostaglandin E2, is part of the signal that drives the cell growth linked to the cancer in their experimental system. High levels of neutrophils have also detected in human clinical samples of melanomas.
INFLAMMATION’S LINK TO AGING
Scientists have long suspected that inflammation may be a bigger player than we thought in aging, given its link to many diseases seen in older people that are known to shorten lifespan.
In fact, chronic low-grade inflammation may be the main reason we age. According to researchers at Newcastle University, inflammation triggers deterioration of cells and the release of destructive molecules, including oxygen free radicals or reactive oxygen species (ROS), which have been linked to the aging process.
The lead of the Newcastle University study, Thomas von Zglinicki, Professor of Cellular Gerontology at the Institute for Aging, said, “There is also a darker side to inflammation: while we become older, a mild form of inflammation without any obvious cause becomes increasingly frequent and ultimately chronic. While this chronic inflammation doesn’t obviously hurt, it still releases the same powerful messenger molecules that cause the pain and fever in the acute situation.”
It turned out these messengers damage cells, especially DNA, which limits the regenerative capacity of multiple tissues in mice, thus accelerating aging.
“People age differently, some much faster than others. We know already that faster aging is often associated with activated markers of chronic inflammation. With these results we can now seriously start thinking about inflammation as a potential driver of accelerated aging and how we might be able to delay it.”
WHAT TO AVOID TO PREVENT CHRONIC INFLAMMATION
It seems that everything you’ve heard about been healthy, such as reducing the amount of processed foods and sugars you eat, exercising and moving more, getting enough sleep and leading a less stressful life helps lower inflammation. But the following are known causes of inflammation that you should avoid or reduce.
- Refined foods, sugars and unhealthy fats
There is endless evidence that a diet heavy in refined foods, sugars and saturated or trans fats is one of the primary causes of chronic inflammation, often via very different mechanisms.Just recently, British scientists found that high levels of saturated fat in the blood may promote damaging inflammation because they encourage white blood cells called monocytes to migrate from the blood into tissues and organs and encourage inflammation. Dr. Kevin Woollard from Imperial College London, who led the research, said, “Modern lifestyles seem to go hand-in-hand with high levels of fat in the diet. This fat comes from the food and drink that we consume; for example, you’d be surprised how much saturated fat a latte contains, and some people drink several through the course of the day. We think that maintaining a relatively high concentration of saturated fats in the diet, for example by constantly snacking on cakes, biscuits and pastries could be causing monocytes to migrate out of the blood and into surrounding tissues.”But consumption of these foods also dumps a lot of sugar into the bloodstream and that, too, has been shown to dramatically increase inflammation markers. A recent Australian study showed that inflammation markers soared just three hours after subjects ate high-glycemic-index foods (refined carbs and sugars and starchy vegetables) that increase the body’s blood sugar levels.The mechanism that links high blood sugar to inflammation may come from the fact that sugars trigger the release of inflammatory messengers called cytokines, according to research published in the American Journal of Clinical Nutrition. High-glycemic-index foods cooked at high temperatures may also trigger the production advanced glycation end-products (AGEs), which have also been shown to increase inflammation. - Omega-6 fatty acids
Omega-6 fatty acids are essential for growth and development, but they need to be consumed in balance with omega-3 fatty acids. When the ratio of omega-6 to omega-3 gets out of control, pro-inflammatory chemicals are produced. The problem is that the Western diet promotes heavy consumption of oils rich in omega-6, such as corn, soybean and safflower oils, as well as things like mayonnaise and salad dressings, all of which skew the omega-6 to omega-3 ratio. - Invisible ingredients
Inflammation is also promoted silently by other ingredients in food, such as emulsifiers that are added to processed foods to enhance texture and extend shelf life. Research published earlier this year by scientists from Georgia State University Institute for Biomedical Sciences found that emulsifiers may alter the gut microbiota and induce intestinal inflammation which, in turn, promotes the development of inflammatory bowel disease and metabolic syndrome. While inflammatory bowel disease is linked to things such as Crohn’s disease and ulcerative colitis, metabolic syndrome is a disorder that’s been linked to type II diabetes and cardiovascular and liver diseases. - Excess weight
Various studies have shown that obesity results in a pro-inflammatory immune response. One study published in the Journal of Clinical Investigation said: “obesity triggers inflammatory pathways in the brain and adipose tissue that dysregulate physiological responses that maintain insulin and leptin sensitivity.” Over time this results in a disastrous storm of side-effects that leads to organ-specific disease and exacerbates systemic insulin resistance, which accelerates the progression toward diabetes, the research said. - Lack of exercise
A study of 4,289 men and women over a 10-year period by researchers from them Department of Epidemiology and Public Health, University College London, found that regular physical activity was associated with lower markers of inflammation and may be important in preventing the pro-inflammatory state seen with aging. Lead researcher Dr. Mark Hamer said, “Physical activity, inflammation, and health are linked together in a complex fashion. Cytokines are secreted transiently in large doses by several metabolically active tissues during exercise, namely from the muscle during contraction and adipose tissue via exercise-related mechanisms.” But paradoxically, regular, long-term exercise was consistently associated with lower levels of systemic inflammatory markers, he said. In other words, exercise that builds muscle results in inflammation in the short term, but reduces it in the long term.Paul Goods, a PhD candidate in exercise physiology from the University of Western Australia, told 24Life that most exercise would cause some muscle damage at the cellular level, which in turn led to an inflammatory response. He added, however, that it’s a necessary part of the muscle adaptation process. “Even very high levels of post-exercise inflammation are generally not considered a negative outcome, as it’s a crucial part of the recovery process, and usually just a reflection of the exercise recently performed. In fact, blunting this post-exercise inflammatory response is ill-advised, from an adaptation point of view.“But there are certainly concerns around inducing high levels of post-exercise inflammation in people who are already chronically inflamed due to other health concerns, and usually more moderate exercise routines will be prescribed for patients who suffer from chronic inflammation. - Disrupted sleep
Poor sleep quality was linked by US researchers to higher levels of inflammation. A study presented to the American Heart Association by Dr. Alanna Morris, a cardiology fellow at Emory University School of Medicine in Atlanta, Georgia, found that participants with poor sleep quality had significantly higher levels of inflammation markers such as fibrinogen, IL-6, and CRP than did participants that slept well. Interestingly, the markers rose dramatically if participants got less than six hours sleep a night. - Stress
Research has shown that anxiety and stress — environmental, mental and physical — appear to generate inflammation because the parts of the brain involved in sensing pain are also activated by stress, generating the pro-inflammatory mediators cytokines. Timothy Olds, Professor of Behavioral Epidemiology at the University of South Australia, says that frequent activation of the human stress response can damage the body in the long run.“Inflammation is good in the short term; it’s the fight or flight response that helps us deal with immediate challenges, but when we are subject to repeated stress we get chronic low-grade inflammation, such as chronic high blood pressure, high blood sugars (which leads to insulin resistance) and the shortening of telomeres [which protect our chromosomes].”
THE C-REACTIVE PROTEIN TEST
If you’re concerned that you may be suffering from chronic inflammation, there is a test you can ask your medical practitioner to carry out, which detects levels of inflammation in your body. It looks at levels of C-reactive protein, regarded as a highly sensitive biomarker of inflammation in the body. The doctor may then suggest pharmacological or lifestyle-related changes to reduce the inflammation.